Acupuncture exerts anesthetic effects and reduces requirements for anesthetic drug use during endoscopic sinus surgery. Researchers from the Shuguang Affiliated Hospital (Shanghai University of Traditional Chinese Medicine) combined acupuncture with general anesthesia. Patients receiving both general anesthesia and acupuncture in a combined treatment protocol had superior patient outcomes compared with patients receiving only anesthetic drugs. The researchers conclude that the addition of acupuncture to a general anesthesia treatment regimen reduces the total dosage requirements for anesthetic drugs and mitigates associated adverse effects. [1]
Researchers (Zhang et al.) used the following study design. A total of 120 patients were treated and evaluated. The patients received endoscopic sinus surgery under general anesthesia. They were randomly divided into an acupuncture treatment group and a control group, with 60 patients in each group. For the control group patients, general anesthesia was administered before and during the operation. The treatment group received acupuncture in addition to the identical anesthesia treatments administered to the drug control group.
The statistical breakdown for each randomized group was as follows. The treatment group was comprised of 34 males and 26 females. The average age in the treatment group was 40 years. The average weight in the treatment group was 64.31 ±5.58 kilograms. The control group was comprised of 31 males and 29 females. The average age in the control group was 38 years. The average weight in the control group was 63.92 ±4.74 kilograms. There were no significant statistical differences in gender, age, and weight relevant to patient outcome measures for patients initially admitted to the study.
For both groups, patients received general anesthesia before the operation. After establishing venous access, 10 ml/kg of Ringer's solution was injected intravenously to maintain circulating blood volume. 30 minutes before anesthesia, 0.01 mg/kg of atropine was given intramuscularly to decrease mucus secretions during anesthesia. Once the anesthesia treatment was initiated, midazolam (0.05 mg/kg), fentanyl (5 μg/kg), propofol (2 mg/kg), and vecuronium bromide (0.1 mg/kg) were injected intravenously.
An oxygen mask and mechanical ventilation were administered. Next, an anesthetic machine was connected to maintain a stable anesthesia delivery per hour through a controlled infusion pump (fentanyl: 5 μg/kg, propofol: 4 mg/kg, vecuronium bromide: 0.05 mg/kg). The blood pressure, heart rate, electrocardiography (ECG), and electroencephalogram (EEG) were monitored. Additional fentanyl and propofol were given based on monitored data.
Acupuncture Treatment
The treatment group patients received one session of acupuncture therapy 30 minutes prior to the induction of general anesthesia. The acupoints used for the treatment group included the following:
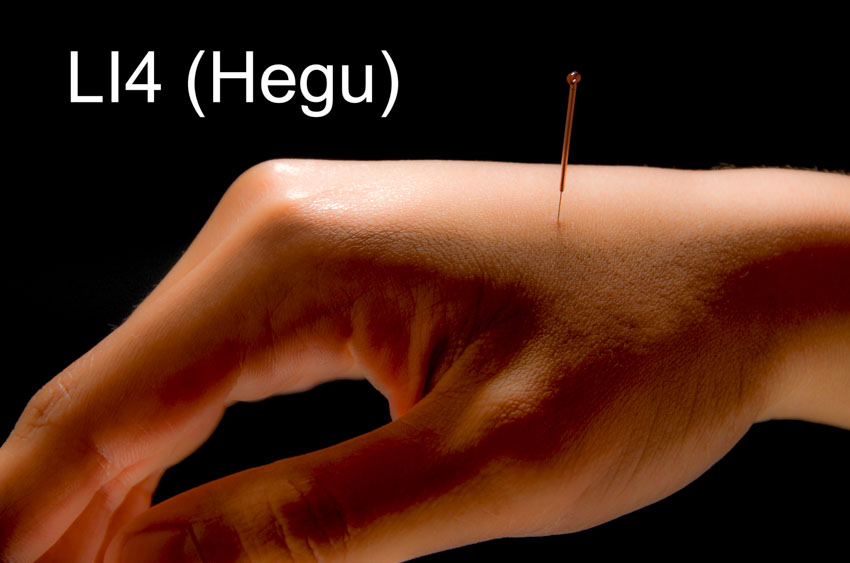
- LI4 (bilateral, Hegu)
- PC6 (bilateral, Neiguan)
Hegu is the yuan-source point of the large intestine meridian. In the Si Zong Xue Ge (Four Principal Acupoints Rhyme), it is written that “Hegu treats diseases in the face and mouth.” Needling Hegu is effective for relieving pain and discomfort in the craniofacial area. Neiguan belongs to the pericardium meridian and is one of the eight confluent points. Modern research confirms that applying electroacupuncture to this point tranquilizes the mind, relieves pain, reduces stress responses to catherterization, and stabilizes blood pressure and heart rate. [2]
Electroacupuncture was applied after the administration of manual acupuncture. Once a deqi sensation was achieved and the Ping Bu Ping Xie (mild tonifying and attenuating) manipulation technique was applied, the acupuncture needles were connected to an electroacupuncture device with a sparse-dense wave. The positive electrode was connected to Neiguan and the negative electrode was connected to Hegu. The frequency was adjusted to 2/100 Hz, with the intensity level set to 8–12 mA or to patient tolerance levels. The needles were retained for 30 minutes once electroacupuncture began.
Evaluations
Multiple subjective and objective instruments were used to measure patient outcomes. First, the additional dosage of fentanyl and propofol used during the anesthesia process was recorded. Second, the heart rate (HR) and the mean arterial pressure (MAP) were calculated. Third, duration of surgery and bleeding volume during surgery were measured. Fourth, pain intensity was scored, using the visual analog scale (VAS), 6 hours after surgery.
The additional dosages of propofol and fentanyl used in the treatment group were 3.18 ±0.24 mg/kg and 2.45 ±0.36 μg/kg respectively, significantly lower than those in the control group, which were 4.25 ±0.37 mg/kg and 3.39 ±0.51 μg/kg. The HR and MAP in the treatment group (78.1 ±4.8 beats/min and 85.4 ±12.1 kPa respectively) had no significant difference compared with those in the control group (76.3 ±5.2 beats/min and 82.2 ±10.7 kPa respectively). There was no significant difference in terms of duration of surgery and bleeding volume in the treatment group (45.73 ±3.20 min, 56.48 ±9.12 ml) and the control group (44.59 ±3.96 min, 60.13 ±11.78 ml). The VAS scores also showed no significant difference between the two groups.
Results
The results indicate that using acupuncture in an integrated treatment protocol significantly reduced the total required dosage of anesthetic medications without compromising anesthetic effects. Zhang et al. conclude that acupuncture is safe and effective for the relief of intraoperative pain for patients receiving endoscopic sinus surgery.
Notes:
[1] Pan LY, Shen HB, Zhang JB, et al. Effects of acupuncture on brain function in patients with
Zhang ZJ, Ma W, Zhang JY, Tong QY. Effect of Electroacupuncture Stimulation on Anesthetic Dosage in Functional Endoscopic Sinus Surgery [J]. Shanghai Journal of Acupuncture and Moxibustion, 2020, 39(05): 576-578.
[2] Liu TY, Yang HY, Chu LX. Current Status and Analysis of Acupuncture Anesthesia [J].Chinese Acupuncture, 2007, 27(12):914-916.


