Acupuncture alleviates pain and restores mobility for patients with temporomandibular disorder (TMD), a temporomandibular joint disturbance syndrome involving the jaw joint and muscles. Second Hospital Affiliated to Fujian University of Traditional Chinese Medicine researchers examined two acupuncture protocols in a clinical trial. They determined that warm needle acupuncture produced a 93.3% total effective rate and standard manual acupuncture produced an 86.7% total effective rate. [1] The efficacy criteria included 4 levels:
- Fully recovered: swelling and painful sensation disappeared, headache and tinnitus disappeared, unrestrained jaw mobility, clicking sound at the jaw disappeared
- Significantly effective: symptoms markedly improved
- Relieved: symptoms slightly improved
- Ineffective: symptoms persisted
Among the 30 patients in the warm needle acupuncture group, 18 cases fully recovered, 7 were significantly effective, 3 were effective, and 2 were ineffective. The total efficacy rate was 93.3%. By contrast, within the manual acupuncture group, 11 cases fully recovered, 10 were significantly effective, 5 were effective, and 4 were ineffective. The total efficacy rate was 86.7%. The data indicates that adding the warm needle protocol increases the total effective rate and the fully recovered rate. Learn more in the acupuncture continuing education course entitlted TMJ Orofacial Pain at HealthCMi.
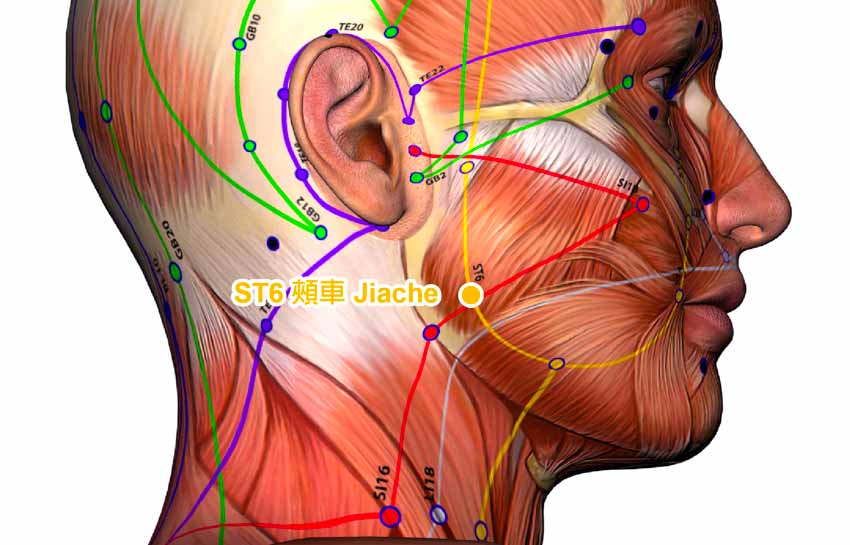
Patients received the same acupuncture treatments with the exception of moxa at ST7 (Xiaguan), GB3 (Shangguan), and SI19 (Tinggong) for patients in the warm needle acupuncture group. Patients took a lateral position to expose the affected area. Filliform needles (2 cun, 28 gauge) were applied at the following acupoints on the affected side:
- ST7 (Xiaguan)
- GB3 (Shangguan)
- ST6 (Jiache)
- SI19 (Tinggong)
In addition, LI4 (Hegu) was applied to the unaffected side. Needles were inserted perpendicularly. Insertion length for Xiaguan, Shangguan, and Tinggong was 1.5 cun, 1.2 cun, and 1.0 cun respectively. Needles at Jiache were threaded towards Xiaguan with a mild reinforcing-attenuating method. Needles were retained after obtaining deqi for at 30 minutes. Moxa were connected to needles on Xiaguan, Shangguan, and Tinggong in the warm needle acupuncture group but not that standard manual acupuncture group. Treatment was given once daily, with 7 days completing the session.
The study used a sample of 60 patients admitted into the hospital from June 2019 to June 2020. The 60 patients were randomly categorized into a manual acupuncture control group and a warm needle acupuncture group, with 30 patients in each group. For the manual acupuncture control group, the mean age was 35.73 ±6.39 years. The mean course of disease was 25.64 ±6.77 days. Twelve patients in this group were males and 18 were females. For the warm needle acupuncture group, the mean age was 34.22 ±5.19 years. The mean course of disease was 23.84 ±7.11 days. Eleven patients in this group were males and 19 were females.
Patients included in the investigation had experienced strain or visible injuries, presented abnormality in jaw movement (difficulty in opening or closing the jaw), suffered clicking sound at the jaw, and pain in one or both of the temporomandibular joints (TMJs). Imaging detection demonstrated widening of the joint space and restrained condylar movement. Patients with head or face injuries, hemorrhagic diseases, or malignant tumors were excluded from the investigation.
A previous study used a similar design and compared 70 temporomandibular joint disturbance syndrome patients in two groups: a warm needle acupuncture group and a drug group (diclofenac sustained release capsules and glucosamine hydrochloride capsules). The results show that the warm needle acupuncture group experienced greater improvements in terms of the Visual Analog Variables score (VAS) and dysfunction index (DI). Six months after the treatment, the efficacy rate of the warm needle acupuncture group was 79%, compared with 47% in the drug control group. [2]
References:
[1] Wang Xuefang, Zheng Xiaoyan, Clinical Observation on Treating Temporomandibular Joint Disturbance Syndrome with Traditional Mongolian Medicine Warm acupuncture, Journal of Chinese Minzu Medicine, July 27, Issue 7, July 2021.
[2] Clinical Observation of Warm Acupuncture on Treating Temporomandibular Joint Disorder Syndrome, Liu Jing, Han Dexiong, Chen Qin, Chinene Journal of Tradional Chinese Medicine and Pharmaceuticals, February 2019, Vol.34, No. 2.