Acupuncture significantly reduces onset frequency, level and duration of pain, and accompanying symptoms in tension type headache (TTH) patients. Researchers from Guanganmen Hospital (affiliated with China Academy of Chinese Medical Sciences) conducted a clinical trial. A special acupuncture point, Yangshang, was used in the treatment protocol for all participants in the medical investigation.
The trial used the special acupuncture point (Yangshang) along with heated needles. The trial compared the efficacy of fire needle acupuncture with manual acupuncture to determine an optimal protocol. The fire needle acupuncture treatment group yielded superior patient outcomes.
Measurement parameters included the Visual Analog Scale (VAS) score for level of pain at T1 (immediately after the treatment course), T2 (one month following the treatment course), and T3 (three months following the treatment course), and a symptom scoring system for pain relief, frequency of onset, as well as duration of pain. The Headache Impact Test (HIT-6) was also employed. After the completion of treatment, the fire needle acupuncture treatment group demonstrated more marked improvements in all measurement parameters. Based on the four-level efficacy rating system used in the study, the efficacy rate was 96.55% for the fire needle group.
The researchers used the following study design. The sample of patients was comprised of 58 cases admitted into the hospital. Patients were randomly divided into two groups. There were no major statistical differences between the two groups at the outset.
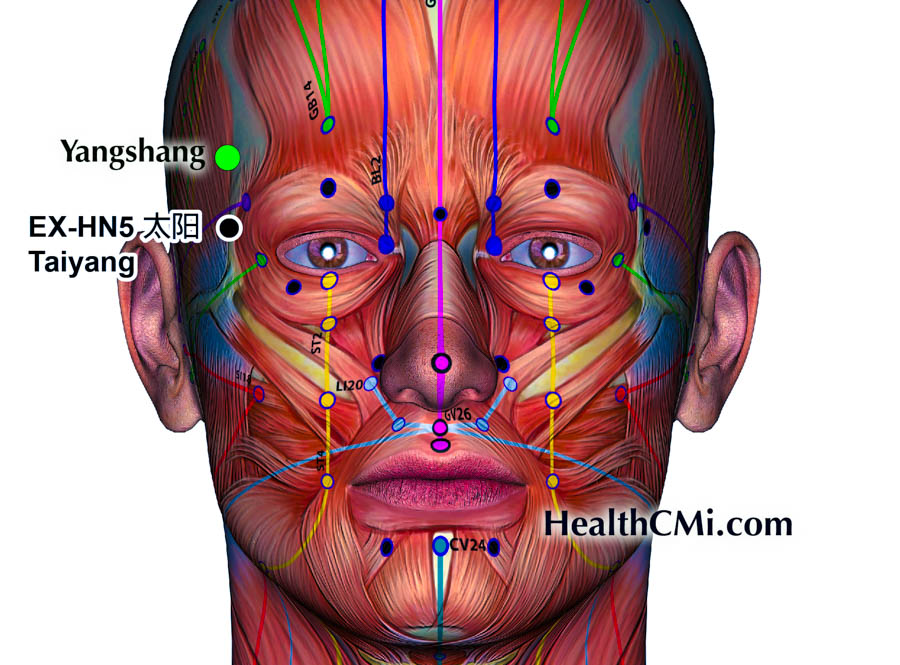
The two groups both received manual acupuncture. For both groups, the main acupoints used in the procedure were Ashi, Yangshang, and Taiyang (EX-HN5). Yangshang point is commonly used by Dr. Huang Shixi from Guanganmen Hospital. It is located 1.2 cun superior to Taiyang next to the hairline. Supplementary points were the following:
- GB20 (Fengchi)
- ST8 (Touwei)
- TE6 (Zhigou)
- LI4 (Hegu)
- LR3 (Taichong)
- SP6 (Sanyinjiao)
Patients took a seated or a supine position. Acupuncture needles (0.35 ×25 mm and 0.30 × 40 mm) were sterilized and inserted into the aforementioned points. For Taiyang, Yangshang, and Ashi, the 0.35 × 25mm needles were heated using an alcohol burner until the needles turned a reddish color. Afterwards, the needles were swiftly inserted to an insertion length of 2 mm and then removed. The next step was to apply the 0.30 × 40mm needles.
- For Ashi points, needles were inserted obliquely to a depth of 0.5 cun.
- For Taiyang, needles were inserted perpendicularly to a depth of 0.5 cun.
- For Yangshang, needles were inserted obliquely to a depth of 0.5 cun.
- For Fengchi, needles were inserted perpendicularly to a depth of 0.5 cun.
- For Touwei, needles were inserted transversely to a depth of 0.5 cun.
- For Zhigou, Hegu, Taichong, Sanyinjiao: needles were inserted perpendicularly to a depth of 0.7 cun.
Mild reinforcing-attenuating manipulation techniques were applied. Needle retention time was 50 minutes. The fire needle acupuncture group received moxa in addition to the above therapy. Upon the arrival of deqi, the needles at Ashi and Yangshang were connected to moxa pieces. The moxa was placed 2.5 cm away from the skin surface.
Treatment was conducted daily, with six consecutive days completing a course. Patients received two courses with a three-day interval between the courses. The researchers comments that the fire needle technique enhanced efficacy by dredging the meridians and collaterals though the warmth of the needle, activating the qi energy, and thereby relieving pain.
A difficulty in this protocol is that two different parameters were changed in the treatment protocol between the fire needle group and the manual acupuncture control group. The fire needle group received the in-out fire needle technique and moxibustion. As a result, the data may reflect increases in efficacy from fire needle therapy or moxibustion or a combination of the two. Additional research with a third arm isolating fire needle therapy from moxibustion would help to clarify parameters of efficacy.
Despite the additional of two variables in the fire needle group, the results are consistent with other pieces of research reviewed by the HealthCMi team. Consistently, electroacupuncture, manual acupuncture, and warm needle acupuncture produce significant effects in the alleviation and prevention of tension headaches across multiple sources of research from independent sources from many nations and universities. As a result, the HealthCMi team endorses acupuncture as a first-line treatment for tension headaches.
Reference:
Sun Shaoxin, Li Shanshan, Bin Lulu, Clinical Observation on Treating Tension-type Headache with Warm acupuncture, China Journal of Clinical Medicine, Volume 51, Issue 1, 2023.


