Acupuncture provides relief from COVID-19 by reducing inflammation. University of Pennsylvania (neurosurgery department) and Tianjin University of Traditional Chinese Medicine researchers determined that acupuncture alleviates respiratory, digestive, cardiovascular, and nervous system disorders associated with COVID-19. [1] In addition, acupuncture was found effective for alleviating fatigue, depression, and insomnia associated with COVID-19.
The research team finds acupuncture successful in regulating inflammation affecting the immune system. The researchers also document the success of acupuncture in regulating oxidative stress levels and neurotransmitter releases. In addition, diseases of the vascular system were alleviated with the application of acupuncture and acupuncture treatments actively regulated mitochondrial function and cardiomyocyte apoptosis. Based on the findings, the researchers indicate the need for further investigations to elucidate the mechanisms of action that acupuncture exerts in patients with COVID-19.
Acupuncture’s ability to improve digestion and alleviate diarrhea, nausea, vomiting, and abdominal discomfort for COVID-19 patients is consistent with other areas of medicine confirming acupuncture’s ability to exert benefits to the digestive system. For example, The American Society of Clinical Oncology formally recommends acupuncture as an effective modality for the treatment of nausea and vomiting due to chemotherapy. Overall, the digestion system findings are consistent across significant meta-analyses published in JAMA. [2, 3] This is especially significant since patients reporting digestive disturbances as the initial symptoms of COVID-19 are most likely to develop into severe cases.
The research team finds that the pain relieving effects of acupuncture and its ability to alleviate fatigue are associated with the ability of acupuncture to regulate neurotransmitter and neuropeptide levels. This is consistent with findings published in BMJ (British Medical Association) and BMC (BioMed Central). [4, 5, 6] These findings are significant because long COVID remains an issue, with many patients having insomnia and mental disorders over six months after discharge. [7] In related standards, the American Cancer Society recommends acupuncture for the alleviation of fatigue due to cancer treatment.
Long COVID as a cause of depression indicates that acupuncture is an important treatment modality. Published in the Annals of Internal Medicine, The American College of Physicians notes that acupuncture combined with antidepressants is a superior protocol versus pharmacological monotherapy. [8] This approach indicates that integrated treatment protocols optimizes patient outcomes.
The research team did a breakdown of the most common acupuncture points used in clinics based on respiratory, digestive, neurological, and mental disorders. For respiratory system disorders including fever, dyspnea, chest pain and tightness, and coughing, the following acupoints were determined to be most common:
- Dazhui (GV14)
- Hegu (LI4)
- Neiguan (PC6)
- Quchi (LI11)
- Dingchuan (EX-B1)
The research is consistent with modern clinical practice. GV14 is one of the single most important acupoints for the alleviation of febrile diseases. It is a point of sea of qi acupoint and is a meeting point of the governing vessel with the six yang channels of the hand and foot. LI4 is commonly used for the invasion of external pathogenic factors and is a yuan-source point, Gao Wu command point, and Ma Dan-yang heavenly star acupoint. PC6 is an important luo-connecting acupoint and is a confluent point of the yin linking vessel. Dingchuan, an extra point translated as calm dyspnea, often provides immediate and long-term relief for wheezing, asthma, dyspnea, coughing, and pain of the back.
Digestive symptoms of COVID-19 include diarrhea, abdominal discomfort and distention, nausea, vomiting, low appetite, and constipation. The most common acupoints documented for the digestive system were:
- Qihai (CV6)
- Guanyuan (CV4)
- Zusanli (ST36)
- Hegu (LI4)
- Sanyinjiao (SP6)
A licensed acupuncturist will immediately recognize the importance of these points because they are textbook examples of acupoints used for digestion improvement. Interestingly, CV6, CV4, and ST36 are combined with CV3 (Zhongji) for the treatment of fatigue and chronic low levels of vitality. This is termed the Dan Tian treatment, named after the area below the navel used in Chinese medicine for the support of vital energy. Exhaustion and intestinal distress may present with long COVID and the inclusion of CV6 and CV4 addresses this concern.
Neurological concerns including headaches, fatigue, anosmia (loss of smell), dysosmia, extremity pain, and dizziness were determined common adverse effects associated with COVID-19. The researchers documented the most common acupoints used for these ailments in COVID-19 patients:
- Mingmen (GV4)
- Zusanli (ST36)
- Hegu (LI4)
- Sanyinjiao (SP6)
- Quchi (LI11)
For mental and psychological disorders associated with COVID-19 (e.g. anxiety, depression, insomnia), the following acupoints were determined the most commonly applied:
- Shenmen (HT7)
- Zusanli (ST36)
- Neiguan (PC6)
- Baihui (GV20)
- Ear Shenmen (auricular point)
The researchers indicate that acupuncture is synergistic with drug therapy. Based on the research team’s findings, acupuncture is an appropriate treatment modality for patients with COVID-19 or its long-term adverse effects.
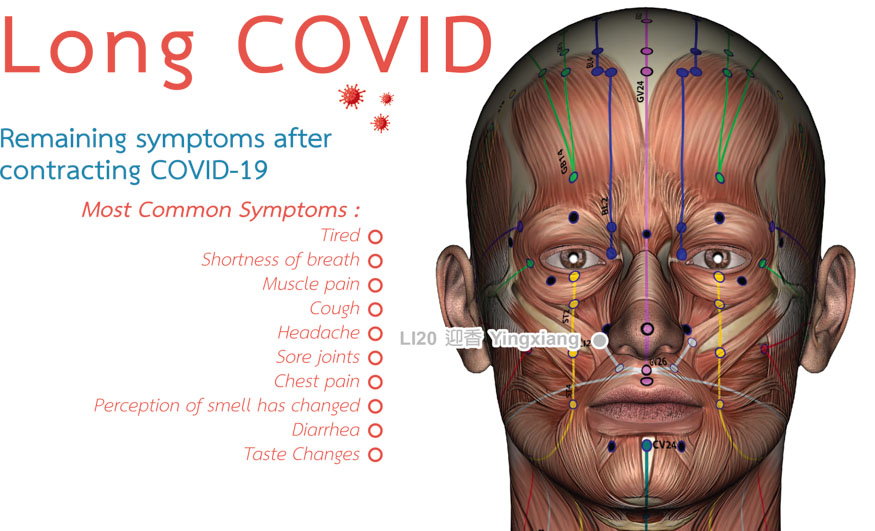
* Illustration depicts LI20 (Welcome Fragrance), used for restoration of taste and smell by licensed acupuncturists.
References:
[1] Wang, Lifen; Hu, Xiyou; Geng, Lianqi; Li, Ningcen; Chen, Yong; Zhang, Jingyu; Yuan, Xinru; Huang, Lihong; Ba, Dongsheng; Lian, Jinyu; Lyu, Xiaoyan; Chen, Zelin; Zhang, Yue; Chen, Bo. Multi-effective characteristics and advantages of acupuncture in COVID-19 treatment. Acupuncture and Herbal Medicine 3(2):p 83-95, June 2023.
[2] Shen J, Wenger N, Glaspy J, et al. Electroacupuncture for control of myeloablative chemotherapy-induced emesis: a randomized controlled trial. JAMA 2000;284(21):2755–2761.
[3] Qi LY, Yang JW, Yan SY, et al. Acupuncture for the treatment of diarrhea-predominant irritable bowel syndrome: a pilot random- ized clinical trial. JAMA Netw Open 2022;5(12):e2248817.
[4] Wang T, Xu C, Pan K, et al. Acupuncture and moxibustion for chronic fatigue syndrome in traditional Chinese medicine: a systematic review and meta-analysis. BMC Complement Altern Med 2017;17(1):163.
[5] Xu S, Yu L, Luo X, et al. Manual acupuncture versus sham acupuncture and usual care for prophylaxis of episodic migraine without aura: multicentre, randomised clinical trial. BMJ 2020;368:m697.
[6] Li X, Dai Q, Shi Z, et al. Clinical efficacy and safety of electroacupuncture in migraine treatment: a systematic review and network metaanalysis. Am J Chin Med 2019;47(8):1755–1780.
[7] Spinner CD, Gottlieb RL, Criner GJ, et al; GS-US-540-5774 Investigators. Effect of Remdesivir vs standard care on clinical status at 11 days in patients with moderate COVID-19: a randomized clinical trial. JAMA 2020;324(11):1048–1057.
[8] Qaseem A, Barry MJ, Kansagara D; Clinical Guidelines Committee of the American College of Physicians. Nonpharmacologic versus pharmacologic treatment of adult patient with major depressive disorder: a clinical practice guideline from the American college of physicians. Ann Intern Med 2016;164(5):350–359.


