Zhuji Disan Renming Hospital researchers conclude that acupuncture combined with herbal medicine is effective for the alleviation of pain and discomfort due to surgical removal of the gallbladder (postcholecystectomy syndrome). A Traditional Chinese Medicine (TCM) treatment group was administered a classic herbal formula (Si Ni San) and a semi-protocolized acupuncture point prescription. The TCM treatment group had a 98.1% total effective rate. A drug control group received conventional drug therapy and had an 85.4% total effective rate. The results demonstrate that the integration of acupuncture and herbal medicine into postoperative protocols produces significant positive patient outcomes. Let’s take a look at the results.
Postcholecystectomy Syndrome (PCS) refers to the presence of pain and discomfort in the upper abdomen after surgical removal of the gallbladder. In China, PCS occurs in about 30 to 40% of patients who undergo cholecystectomy, and 15% of PCS cases are severe cases. Characteristic symptoms include indigestion, nausea, belching, upper abdominal discomfort, upper abdominal distention after eating, abnormal defecation, fatigue, and in severe cases, jaundice and fever. This study focuses on a scientific comparison between drug therapy and acupuncture plus herbs therapy for the treatment of PCS.
The study design was as follows. A total of 100 patients with PCS were treated and evaluated in the study. All patients were diagnosed with PCS between July 2010 and July 2014. They were divided into a control group and a treatment group, with 48 cases in the drug control group and 52 cases in the TCM treatment group.
The statistical breakdown for each randomized group was as follows. The treatment group was comprised of 38 males and 14 females. The average age in the treatment group was 55 (±15) years. The average course of disease in the treatment group was 1.56 (±0.98) years. There were 25 patients who engaged in mental labor and 27 patients who engaged in physical labor. The control group was comprised of 37 males and 11 females. The average age in the control group was 45 (±16) years. The average course of disease in the control group was 1.07 (±0.87) years. For occupations, there were 21 patients who engaged in mental labor and 27 patients who engaged in physical labor. There were no differences in terms of age, course of disease, and type of job relevant to patient outcome measures.
The treatment group received electroacupuncture and herbal treatment. For electroacupuncture, the following acupoints were selected:
- BL18 (Ganshu)
- BL19 (Danshu)
- BL20 (Pishu)
- BL21 (Weishu)
- BL22 (Sanjiaoshu)
- BL23 (Shenshu)
- BL25 (Dachangshu)
- Dannang (Ashi)
- ST36 (Zusanli)
- ST37 (Shangjuxu)
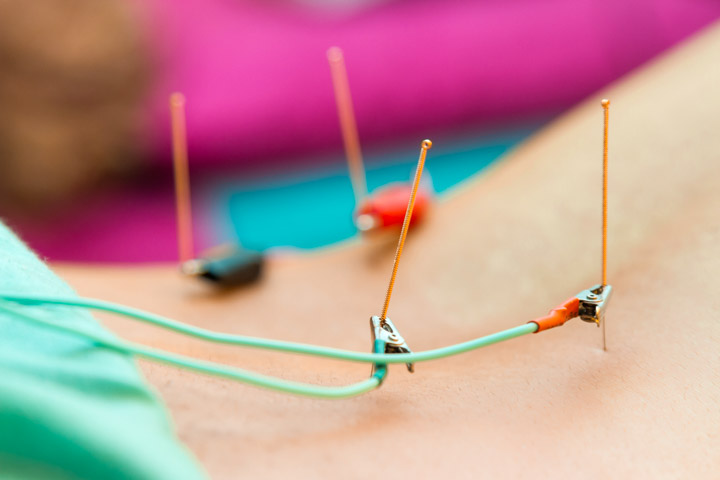
- GB34 (Yanglingquan)
Treatment commenced with patients in a prone position. After disinfection of the acupoint sites, a 0.30 mm x 40 mm disposable filiform needle was inserted into each acupoint with a high needle entry speed. The needle was lifted (with a heavy force), thrust (with a light force), and rotated (with a heavy force). Once a deqi sensation was obtained, electroacupuncture was applied. A continuous wave of 2 Hz was applied with an intensity level set to patient tolerance levels. Electroacupuncture was applied once per day, 30 minutes per acupuncture session, 7 days per treatment course, for a total of 3 treatment courses.
In addition, a modified version of the herbal formula Si Ni San was administered. Patients consumed the TCM (Traditional Chinese Medicine) decocted herbs once daily, 7 times per treatment course, for a total of 3 treatment courses. The ingredients of the modified herbal formula were as follows:
- Chai Hu 10g
- Bai Shao 20g
- Zhi Ke 9g
- Bai Dou Kou 6g
- Yu Jin 10g
- Chuan Hou Po 10g
- Da Huang 10g
- Gan Cao 10g
- Chao Bai Zhu 9g
- Chi Fu Ling 9g
Additional herbs were prescribed according to specific diagnostic considerations. For liver-stomach disharmony, the following herbs were added:
- Huang Lian 6g
- Ban Xia 10g
- Guang Mu Xiang 10g
For spleen deficiency, the following herbs were added:
- Ren Shen 10g
- Chen Pi 10g
- Shao Yao 10g
For liver-stomach damp-heat, the following herbs were added:
- Shan Zhi 10g
- Yin Chen 10g
- Ze Xie 10g
The drug control group was given Xiaoyan Lidan tablets (oral herbal medication for resolving inflammation and benefiting the gallbladder) or ursodeoxycholic acid tablets. For the Xiaoyan Lidan tablets, the dosage was 6 tablets, 3 times per day. For the ursodeoxycholic acid tablets, the dosage was 100 mg, 3 times per day. In addition, patients received ofloxacin, an antibiotic. Ofloxacin capsules were orally administered, 0.2 g each time, 3 times per day, 7 days per treatment course, for a total of 3 treatment courses. Notably, antispasmodics and analgesics were also prescribed for patients in the drug control group when pain became very serious. Patients in both groups were advised to maintain a positive emotional state and to avoid taking spicy food and becoming exhausted.
The total treatment effective rate for each patient group (TCM treatment and drug control) was derived as the percentage of patients who achieved at least an effective treatment tier of improvement. The treatment efficacy for each patient was categorized into 1 of 3 tiers:
- Recovery: Complete or significant absence of symptoms.
- Effective: Symptoms showed improvement.
- Not effective: Symptoms showed no visible improvement.
The acupuncture and herbal medicine treatment group achieved a total effective rate of 98.1%. The drug control group achieved a total effective rate of 85.4%. The combination of acupuncture plus herbs outperformed drug therapy.
In Traditional Chinese Medicine, PCS falls under the following classes of disorders: xietong (rib-side pain), weiwantong (stomach duct pain), xinji (heart palpitations), and huandan (jaundice). The root cause of PCS is liver qi stagnation. Thus, the treatment principle of this problem is to course the liver and fortify the spleen, and to activate qi and blood circulation. Si Ni San was first mentioned in the Shang Han Lun, where it is indicated for liver qi stagnation and counterflow qi. Principle signs would be those of liver qi stagnation, hypochondriac pain, or abdominal pain.
The researchers selected Beishu (Back Shu) and He-Sea acupoints for the treatment of PCS. Many of the acupoints are specifically indicated for benefitting major internal organs and digestion. The TCM treatment principles were to course the liver and gallbladder qi, invigorate blood, dispel blood stasis, disperse swelling, and alleviate pain. The investigation results demonstrate that a combination of herbs and acupuncture are beneficial to PCS patients and produce significant positive patient outcomes.
Reference:
Sheng YX et al. Therapeutic Observation of Acupuncture plus Chinese Medication for Postcholecystectomy Syndrome [J]. Shanghai Journal of Acupuncture and Moxibustion, 2016, 35(3):291–293.


