Acupuncture exerts anesthetic effects, alleviates pain, and reduces gingival bleeding during and after dental procedures. Three independent investigations confirm the findings. In one study, acupuncture outperformed a local anesthetic and produced better anesthetic effects. Two other investigations find acupuncture effective for the alleviation of pain and conclude that acupuncture significantly reduces copious gingival bleeding during and after tooth extraction.
Hunan University of Traditional Chinese Medicine researchers compared the anesthetic effects of acupuncture and a local anesthetic during tooth extraction. The results of the controlled clinical trial find acupuncture more effective than compound articaine hydrochloride injections. [1]
The university researchers (Pan et al.) used the following study design. A total of 60 subjects participated in the study. Patients were from the Dentistry Department of the First Affiliated Hospital of the Hunan University of Traditional Chinese Medicine. Randomization into an acupuncture treatment group and a control group, with 30 subjects in each group, was employed. For control group patients, compound articaine hydrochloride injections were administered before tooth extraction.
Compound articaine hydrochloride injection is a sterile and aqueous solution containing articaine (4%) and epinephrine (1:100,000), both commonly used during dental procedures. The treatment group received only acupuncture. The criteria for the treatment group patients were the following:
- Ages between 18-65 years
- Consistent with the indication of tooth extraction (i.e., severe caries, malopposed or malpositioned teeth, impacted wisdom teeth, severe periapical or periodontal diseases, severe oral soft and hard tissue diseases
- Informed consent was signed for each patient
The following exclusion criteria were applied:
- Malignant systemic diseases such as hemophilia, aplastic anemia, thrombocytopenic purpura, and leukemia
- Severe comorbid hypertension, heart disease and other cardiovascular diseases
- Severe comorbid diseases affecting major organs
- Acute infectious diseases, acute mucosal inflammation, oral malignant tumors
- Pregnant or lactating women
- Women during menstrual cycle
The statistical breakdown for each randomized group was as follows. The treatment group was comprised of 18 males and 12 females. The average age in the treatment group was 42 ±14 years. The control group was comprised of 17 males and 13 females. The average age in the treatment group was 47 ±15 years. There were no significant statistical differences in gender, age, and other demographic factors relevant to patient outcome measures for patients initially admitted to the study.
Acupuncture And Drug Groups
For the control group, 1.0 ml of compound articaine hydrochloride injection was administrated with a local anesthetic syringe before dental surgery. If pain became severe during operation, another 0.5 ml of compound articaine hydrochloride injection was given. The total time and amount of additional anesthetic injection was recorded. The primary acupoints selected for the treatment group were the following:
- LI4 (Hegu)
- ST44 (Neiting)
- ST7 (Xiaguan, the surgical side)
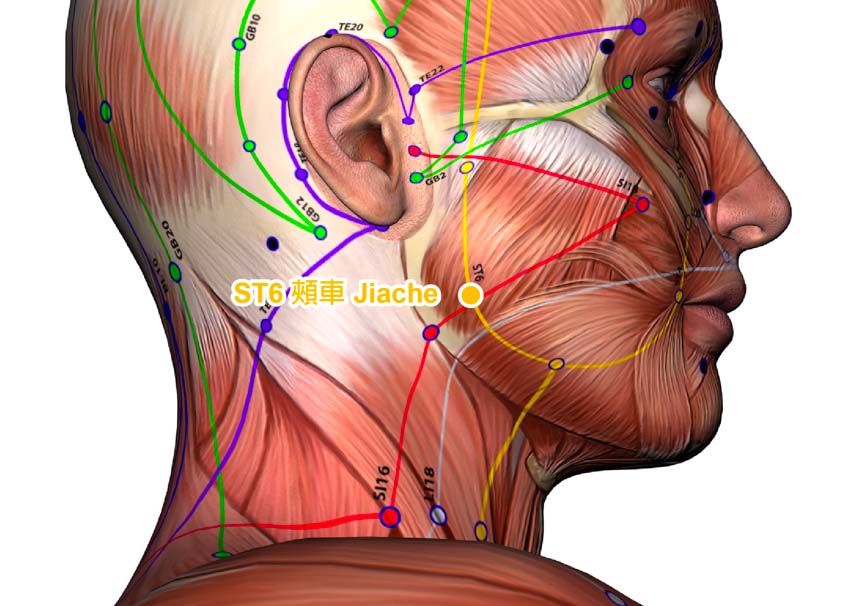
- ST6 (Jiache, the surgical side)
- For the extraction of incisors and canine teeth, CV24 (Chengjiang) on the surgical side was also added.
Treatment commenced with patients in a supine position and at mouth opening. After disinfection of the acupoint sites, a 0.35 mm x 40 mm disposable filiform needle was inserted into each acupoint with a high needle entry speed. For Hegu and Neiting, the needles were twisted, lifted, and thrust for 2 minutes (90 degrees, 180 r/min), after reaching a standard depth and a deqi sensation was obtained. For Xiaguan, Jiache, and Chengjiang, the needles were inserted to a depth of 15–25 mm; next, the needles were manipulated to obtain a deqi sensation. Then, the needles were gently pulled until they reached the subcutaneous tissue. The needles were retained until 10 min after tooth extraction or when there was no obvious pain.
If pain became severe during the operation, the needles at each point were manipulated for 1 minute. If pain was not relieved after manipulation was applied, 0.5 ml of compound articaine hydrochloride injection (identical to that used by the control group) was given. The total time and amount of additional local anesthetic injection should was recorded.
Acupoint Selection
Acupuncture points selected for the study were based on Traditional Chinese Medicine principles. Hegu is the Yuan-source point of the Hand Yangming Large Intestine meridian. In the Sizong Gejue (Song of the Four Command Points), it is noted that "Hegu (LI4) regulates the face and mouth." In the Zhengjiu Jiayi Jing (Systematized Canon of Acupuncture and Moxibustion), it is noted, “Hegu is indicated for tooth pain.”
Neiting is the Ying-spring point of the Foot Yangming Stomach meridian. According to the Zhengjiu Jiayi Jing, needling this point treats “lower tooth pain.” The researchers conclude that “Needling aucpoints on the Hand and Foot Yangming meridians are effective for relieving tooth pain.” In Traditional Chinese Medicine, the Hand Yangming Large Intestine meridian enters the lower gums and the Foot Yangming Stomach meridian enters into the upper gums. Xiaguan and Jiache are located on the Foot Yangming Stomach meridian.
The deep anatomical structure of the Xiaguan point includes trigeminal nerve branches (i.e., the maxillary nerve, auriculotemporal nerve). The deep anatomical structure of the Jiache point includes the facial nerve, great auricular nerve, and the masseteric nerve. These points are traditionally indicated for the treatment of tooth pain.
Evaluations
Multiple subjective and objective instruments measured patient outcomes. First, the general condition was recorded, including blood pressure, heart rate, respiratory rate, operation duration, the amount of bleeding during tooth extraction, and the total time and amount of additional local anesthesia injections. Second, the anesthetic effective rate was evaluated according to the National Anesthetic Scoring Standard:
- Class I (super excellent): patients stay quiet and feel no pain during operation
- Class II (excellent): patients stay quiet and feel occasional pain during operation
- Class III (good): patients feel obvious pain and additional anesthesia is needed to continue with surgery
- Class IV (bad): pain is so obvious that surgery cannot be continued unless the anesthesia method is changed.
Third, the improvement of pain intensity was scored using the pain rating index (PRI) and the visual analog scale (VAS). Fourth, the adverse effect (e.g., dizziness, palpitations, nausea) rate was recorded.
Results
After completion of treatments, the acupuncture group reported 25 cases of Class I (83.4%), 4 cases of Class II, 1 case of Class III, and 0 cases of Class IV. The treatment group reported 24 cases of Class I (80.0%), 4 cases of Class II, 2 cases of Class III, and 0 cases of Class IV. The amount of bleeding during surgery as well as the adverse effect rate in the acupuncture group was significantly lower than in the control group (p<0.01, p<0.05).
The acupuncture group produced a 2.42 ±0.78 ml of average bleeding with an adverse effect rate of 6.7%. The control group produced a 3.20 ±0.86 ml of average bleeding with an adverse effect rate of 30.0%. There were no significant differences between the two groups regarding other parameters measured in the study (e.g., blood pressure, heart rate, respiratory rate, operation duration, the total time and amount of additional local anesthesia, PRI score, VAS scores).
Nanjing Jiangning District Hospital TCM
Nanjing Jiangning District Hospital of Traditional Chinese Medicine researchers (Xie et al.) had similar results in their independent investigation, published in the Henan Traditional Chinese Medicine Journal. [2] The researchers determined that acupuncture produced an anesthetic effect during tooth extraction. Among 32 patients receiving acupuncture treatments, 24 (75%) patients had Class I results, 6 (19%) patients had Class II results, and only 2 (6%) patients had Class III or IV results. The primary acupoint used in the study was Hegu (LI4). Additional acupoints were added for specific diagnostic considerations. For extraction of upper frontal teeth, the following acupuncture points were added:
- ST2 (Sibai)
- LI20 (Yingxiang)
- GV26 (Renzhong)
For extraction of upper posterior teeth, the following acupuncture points were added:
- ST7 (Xiaguan)
- SI18 (Quanliao)
- ST6 (Jiache)
For extraction of lower frontal teeth, the following acupuncture points were added:
- CV24 (Chengjiang)
- ST5 (Daying)
- ST6 (Jiache)
For extraction of lower posterior teeth, the following acupuncture points were added:
- ST7 (Xiaguan)
- ST6 (Jiache)
- ST4 (Dicang)
Acupuncture needles were inserted into each acupoint with a high speed. After insertion, the needles were lifted, thrust, and twisted to achieve a deqi sensation. The needles were retained until operation completion. Tooth extraction started 5–10 minutes after needle retention.
Shanxi Datong University
Shanxi Datong University researchers investigated the benefits of acupuncture for the treatment of copious gingival bleeding after tooth extraction. [3] Their investigation included patients meeting the following inclusion criteria:
- Underwent tooth extraction and failed to stop bleeding 24 minutes after operation completion
- Bleeding could not be stopped after using other outpatient bleeding control measures
- The cause of bleeding was gingival laceration
The primary acupoints used in the investigation were the following:
- LI4 (Hegu)
- LU6 (Kongzui)
- LI11 (Quchi)
- ST41 (Jiexi)
- LV2 (Xingjian)
- ST44 (Neiting)
- ST36 (Zusanli)
- GV23 (Shangxing)
- ST6 (Jiache)
- ST7 (Xiaguan)
The researchers cited the ancient historical roots and modern research behind the acupoint protocol used in the study. In Traditional Chinese Medicine, gingival bleeding is caused by instability of meridian qi in the yangming meridians. Hegu is the Yuan-source point of the large intestine meridian. Quchi is the He-sea point of the same meridian. Jiexi is the Jing-river point of the stomach meridian. These three distal points combined with the two local points (Jiache, Xiaguan) drain excessive meridian qi and clear stagnant heat of the yangming meridians. In modern terminology, these Chinese medicine principles correlate to regulating autonomic nervous system outflows and reducing inflammation in the local region.
Kongzui is the Xi-cleft point of the Hand Taiyin Lung meridian. Xi-cleft points are places where qi and blood of the meridians are deeply gathered. According to Traditional Chinese medicine, Xi-cleft points of the Yin meridians are indicated for bleeding diseases, while that of the Yang meridians treat acute diseases. [4] In the Zhenjiu Zisheng Jing (Acupuncture Life-Promoting Canon), which was written in the Song dynasty, it is noted that “Needling Kongzui treats spitting of blood.” Modern research confirms that Kongzui is effective for bleeding control. For example, Liu et al. conclude that acupuncture at Kongzui activates sympathetic nerves to release norepinephrine, leading to contraction of blood vessels. Kongzui also increases the content of thromboxane (a hormone released from platelets) in tissue, thereby enhancing blood coagulation and promoting hemostasis. [5]
Xingjian is the Ying-spring point of the Foot Jueyin Liver meridian. Needling Xingjian drains liver qi and clears fire. Neiting is the Ying-spring point of the stomach meridian. Zusanli is the He-sea point of the same meridian. Needling the two acupoints stops bleeding by clearing fire and regulating qi. Shangxing is located on the Du meridian (Governing Vessel). This point is traditionally indicted for gingival bleeding. Needling this point clears heat in the Du meridian.
After disinfection of the acupoint sites, a 0.25 mm x 40 mm disposable filiform needle was inserted into each acupoint with a high needle entry speed. Hegu, Neiting, and Jiache were inserted perpendicularly to a depth of 0.5 cun. Kongzui was inserted perpendicularly to a depth of 1 cun. Xingjian was inserted obliquely and upward to a depth of 1 cun. Zusanli was inserted perpendicularly to a depth of 2 cun. Shangxing and Xiaguan were inserted transversely to a depth of 0.5 cun. Upon arrival of a deqi sensation, the Ping Bu Ping Xie (mild attenuating and tonifying) manipulation technique was applied. A needle retention time of 60 minutes was observed.
Evaluations were made after completion of treatment and in a 3-day follow-up examination. The amount of bleeding in 47 out of 48 patients significantly reduced in the first 5-10 minutes after treatment completion. The bleeding stopped within 20 min. and there was no recurrence of bleeding within a 30-minute observation time after treatment completion. In addition, there was no recurrence of bleeding in the follow up examination. One out of 48 patients had a small amount of bleeding at 20 min. after treatment completion. The bleeding stopped after closing the surgical wound with sutures. There was no recurrence of bleeding in the follow up examination.
The Takeaway
Independent investigations indicate that acupuncture is an important anesthetic and treatment option in dental procedures. Acupuncture exerts an anesthetic effect during tooth extraction and eliminates copious gingival bleeding after operation completion. Common protocols involve the application of acupoints on the Foot Yangming Stomach meridian (e.g., Neiting, Xiaguan, Jiache) and the Hand Yangming Stomach meridian (e.g., Hegu, Quchi). Patients are encouraged to contact local licensed acupuncturists and dental professionals to consult about treatment options.
Notes
[1] Pan J, Lin BL, Chen M, Zhang W, Lou BD. Effects of tooth extraction under acupuncture anesthesia [J]. Chinese Acupuncture and Moxibustion, 2017,37(06):643-646.
[2] Xie H. Observation on acupuncture combined with acupressure anesthesia for extraction and pain relief in 32 cases [J]. Henan Traditional Chinese Medicine, 2011,31(02):183-184.
[3] Zhang HY, Liu BY, Bai ZJ, Guo MF, Lu XZ. Analysis of therapeutic effect of acupuncture treatment in 48 patients with gingival lacerated hemorrhage after tooth extraction [J]. Journal of Shanxi Datong University (Natural Science), 2018,34(06):41-42+50.
[4] Chen et al. Pattern-differentiation treatment of 45 cases of bronchiectasis hemoptysis [J]. Shaanxi Journal of Traditional Chinese Medicine, 1997, 18(4): 163.
[5] Liu et al. Mechanism study and clinical observation on the treatment of hemoptysis after acupoint injection at Kongzui [D]. Zhejiang University of Traditional Chinese Medicine, 2001.


