
Acupuncture is effective for the treatment of migraines. Researchers from Harvard Medical School, Xidian University, and Capital Medical University find acupuncture effective for the reduction of migraine attacks. They discovered that a patient’s pre-treatment brain structure is predictive of the success rate achieved by acupuncture for the reduction or elimination of migraines. [1] Using MRIs and machine learning, specific patterns in brain gray matter prior to treatment were correlated with improved response rates to treatment.
Patients received three acupuncture treatments per week for a total of four weeks. Each acupuncture treatment lasted for a total of thirty minutes. The acupuncture points applied to all patients were the following:
- GV20 (Baihui)
- GV24 (Shenting)
- GB13 (Benshen)
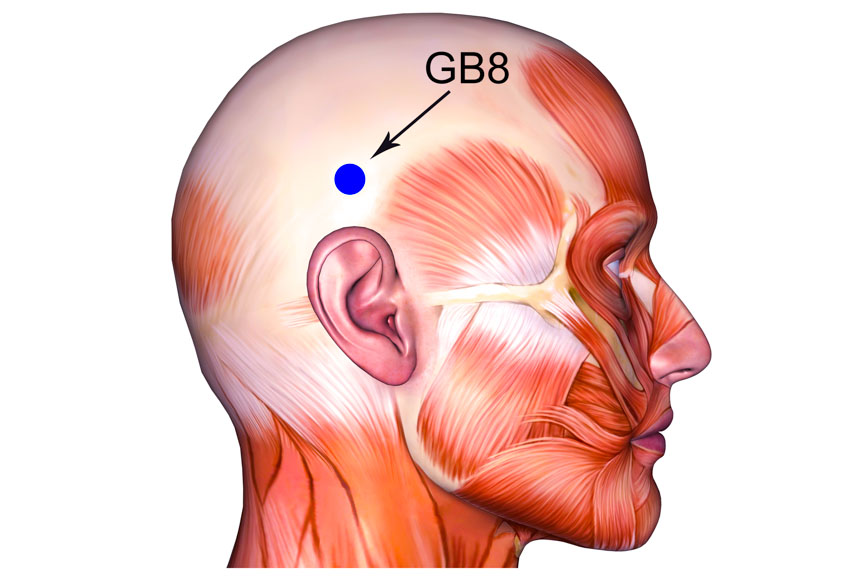
- GB8 (Shuaigu)
- GB20 (Fengchi)
Patients receiving acupuncture were treated with sterile, filiform, single-use Hwato brand acupuncture needles (0.25 × 25 mm). The treatment group was compared with a sham acupuncture group to provide proper controls for the clinical trial. A Healthcare Medicine Institute (HealthCMi) review of the acupuncture needle choice underscores that the needles were 100% metal without any silicone coating. HealthCMi microscopy confirms that the acupuncture needles used in the study were made in the all-metal traditional filiform needle design with the pine cone tip formation.
The investigators used a Siemens 3T MRI system. Data processing was achieved with a human neuroimaging system employing Statistical Parametric Mapping, which is a spatial process used for analysis of fMRIs. Voxel-based morphometry was used to determine differences in gray matter.
A total of 41 patients in the true acupuncture treatment group were included in the analysis. Responders were defined as having at least a 50% reduction in the number of days with a migraine. After four weeks of acupuncture treatment, 19 patients were responders. The researchers determined that all patients had similar pre-treatment baseline gray matter volumes in the cuneus, parietal, and frontal gyri. However, responders had pre-treatment similarities (longitudinal increases) in the left cuneus. Based on the findings, the researchers conclude that MRIs are potentially useful predictors of acupuncture patient outcome rates.
This highlights a way to predict acupuncture’s effectiveness as a treatment method for the resolution or management of migraines, which afflict over 1 billion people every year. It is estimated that migraines are the number one cause of disability in patients ages 15–49. [2] Notably, after four weeks of acupuncture treatment, responders had significantly fewer days with migraines. There were 19 responders and 22 non-responders.
The researchers note that treatment personalization is an “important trend” in medicine. They suggest that MRIs may contribute to determining patient outcomes. The data-driven machine learning process used in the investigation had an 83% accuracy rate in determining responders from non-responders. They indicate that the MRI screening method may help to improve the cost-effectiveness of access to care.
A HealthCMi acupuncture continuing education analysis of the study finds several limitations. Although a careful biomedical screening for patients with migraines was used, there lacked any traditional Chinese medicine differential diagnostics regarding either patient intake or treatment. This may have contributed to a significant underestimation of the success rate of acupuncture therapy.
Prof. Jeffrey Pang, L.Ac. (HealthCMi author & Five Branches University department chair of internal medicine) notes that traditional Chinese medicine pattern differentiation (bian zheng) and biomedical disease differentiation (bian bing) are both important and relevant to treatment parameters. Bian zheng is based on Chinese medicine principles (e.g., zang-fu syndromes, 8 parameters, 6 stages, 4 levels, channel diagnostics, san jiao disorders, and qi, blood, & fluid disorders). Bian bing refers to naming a specific disease based on location or other etiology by disease differentiation (e.g., migraine, cluster headache, tension headache, sinus headache, post-traumatic headache).
Only one acupuncture treatment protocol was used, with a fixed set of acupuncture points for all patients. In an actual acupuncture clinic, specific presentations and diagnostic considerations are used to modify primary and secondary acupuncture point selections and needle techniques. This often contributes to improved patient outcome rates. Common acupuncture points indicated for the treatment of headaches were not part of the study protocols, including: LI4 (Hegu), LV3 (Taichong), ST8 (Touwei), TB5 (Waiguan), BL60 (Kunlun), Anmian (N-HN-54).
The lack of traditional Chinese medicine diagnostics and a fixed set of acupuncture points are not unusual in acupuncture investigations. This is often an issue of funding, timing, and resources. Multi-arm studies often include additional modalities including micro-acupuncture, electroacupuncture, moxibustion, Chinese medicine dietetics, Tui-na massage, and Chinese herbal medicine.
References:
1. Yang, X.J., Liu, L., Xu, Z.L., Zhang, Y.J., Liu, D.P., Fishers, M., Zhang, L., Sun, J.B., Liu, P., Zeng, X. and Wang, L.P., 2020. Baseline Brain Gray Matter Volume as a Predictor of Acupuncture Outcome in Treating Migraine. Frontiers in Neurology, 11, p.111.
Author Affiliations:
Department of Neurology, Beth Israel Deaconess Medical Centre and Harvard Medical School (Boston, Massachusetts).
Engineering Research Center of Molecular and Neuro Imaging of Ministry of Education, Xidian University.
Beijing Hospital of Traditional Chinese Medicine, Capital Medical University.
China Academy of Chinese Medical Sciences.
2. GBD 2016 Headache Collaborators. Global, regional, and national burden of migraine and tension-type headache, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. (2018) 17:954–976.


