
Acupuncture is effective for the treatment of PTSD, especially in combat veterans. In a high-quality placebo controlled clinical trial, researchers conclude that true acupuncture produces moderate to large beneficial clinical and biological outcomes for combat veterans with PTSD. Improvements were significant for the reduction of overall symptom severity and for large scale extinction of fear and startle responses. [1]
The researchers were from the Tibor Rubin VA Medical Center (Long Beach, California), George Washington School of Medicine & Health Sciences (Department of Psychiatry and Behavioral Sciences, Washington, DC), University of California (Department of Medicine, Health Policy Research Institute and General Internal Medicine, Irvine), Analydata (San Diego, California), Yo San University of Traditional Chinese Medicine (Los Angeles, California), Wayne State University School of Medicine (Department of Psychiatry and Behavioral Neurosciences, Detroit, Michigan), and the Susan Samueli Integrative Health Institute (University of California, Irvine). The researchers completed a a two-arm, prospective blinded, randomized clinical trial with parallel groups and tested true acupuncture versus sham acupuncture using placebo controls.
Sham acupuncture was delivered with superficial insertion 2 cm away from true acupuncture points. Relatively little needle stimulation was applied to the sham acupuncture and the sham electroacupuncture device did not stimulate the acupoints but instead simply had a blinking light to present the appearance of functioning. Based on the data, the researchers conclude that true acupuncture is clinically efficacious and improves the psychobiology of combat veterans with PTSD. They add that sham acupuncture is not effective, which indicates the clinical importance of true acupoint functional specificity.
The participants received 1 hour treatments, two times per week, for up to a maximum of 24 treatments over a 15 week period.. Only true acupuncture produced significant overall symptom improvements and fear extinction. Outcomes were measured using the Clinician-Administered PTSD Scale-5 (CAPS-5) and the fear-potentiated startle response assessments. The assessments and treatments were at the Tibor Rubin VA Medical Center (Long Beach, CA). A total of 93 combat veterans with PTSD (18–55 years of age) were randomized into true acupuncture and sham acupuncture groups. A total of 71 patients completed the study.
Acupuncture Treatment
Three separate investigations helped in the development of the acupuncture treatment protocol for the war combatant PTSD study. The first investigation helped to classify PTSD in terms of traditional Chinese medicine (TCM) principles and a second investigation developed the principles into an acupoint prescription, and another investigation implemented the acupoint prescription.
Researchers from the University of New Mexico (Department of Family and Community Medicine) in Albuquerque conducted research to determine TCM diagnostics for PTSD consistent with the American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV). The research team examined accepted literature, interviewed 20 experienced licensed acupuncturists, and used assessments of 21 patients afflicted with PTSD. They conclude that PTSD falls into several TCM patterns, based partly on Chinese medicine principles for insomnia, depression, and anxiety. The primary patterns are the following:
- Heart shen disturbance caused by heat, fire, or deficiency
- Liver qi stagnation
- Kidney deficiency
Next, the researchers determined secondary patterns caused by chronic PTSD affecting health over the long-term of the illness. The following are the related TCM patterns:
- Liver qi stagnation
- Liver overacting on spleen & stomach
- Liver fire
- Phlegm fire
- Phlegm-Dampness
- Heart fire
- Heart, kidney, and spleen organ deficiency [2]
Based on the University of New Mexico research, another investigation worked the diagnostic patterns into a standard treatment protocol for use in research. [3, 4] The researchers that were the first to implement this protocol were from the University of Louisville School of Medicine (Department of Psychiatry and Behavioral Sciences and Family and Geriatric Medicine, Louisville), the University of New Mexico School of Medicine (Department of Family and Community Medicine, Albuquerque) and the Oregon College of Oriental Medicine (Portland). The research was supported by a grant from the USA National Institutes of Health (National Center for Complementary and Alternative Medicine).
The research team created alternating ventral and dorsal acupuncture treatments to avoid tolerance due to frequent use. Electroacupuncture was applied to a flexible selection of two acupoint pairs in either the ventral (supine) or prone (dorsal) treatments with an intermittent pulse of 2/100 Hz. The ventral acupoints were the following:
- LV3
- PC6
- HT7
- ST36
- SP6
- Yintang
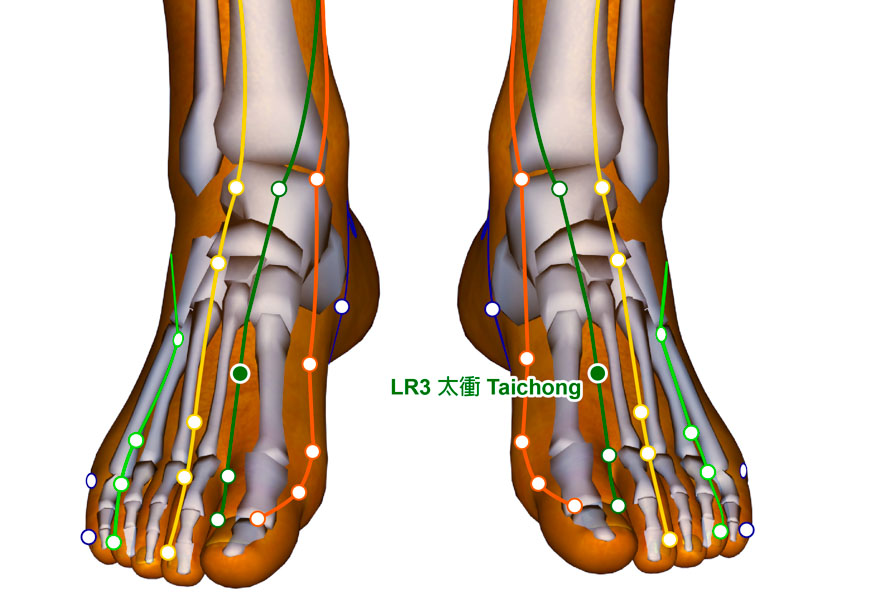
The usage is as follows for the ventral primary points. HT7, PC6, and Yintang are applied for heart shen disturbances, all with peaceful (even) needling technique. LV3 and PC6 are applied for liver qi stagnation, with the peaceful technique. For cases with underlying qi and blood deficiency, the peaceful technique is applied to ST36 and SP6. The dorsal acupoints were the following:
- GB20
- BL14
- BL15
- BL18
- BL20
- BL21
- BL23
The usage of the dorsal points is as follows. BL14 and BL15 were applied with the peaceful technique for heart shen disturbances. GB20 and BL18 were applied with the peaceful technique for liver qi stagnation. BL23 was applied with the reinforcing technique for kidney deficiency. BL20 and BL21 were applied with the peaceful technique for qi and blood deficiency.
Additional secondary acupoints were included in the protocol of which 3 of them could be flexibly prescribed per session. Ventral secondary points were matched with ventral primary acupoints and the same for dorsal acupoints. The following is a list of the available secondary points and the techniques applied to them based on pattern diagnostic presentation:
- Liver overacting on spleen, reinforcing: LV13, BL18, BL20
- Liver overacting on stomach, reducing: LV14, BL18, BL21
- Stomach fire, reducing: ST44, GV14, BL21
- Liver fire, reducing: LV2, GV14, BL18
- Hot phlegm, reducing: ST40, GV14, BL21
- Phlegm dampness, reducing: SP9, BL20
- Heart yin and blood deficiency, reinforcing: HT6, BL17, BL15
- Spleen qi and yang deficiency, reinforcing: SP3, BL20, BL23
- Kidney yin or jing deficiency, reinforcing: KD6, BL52, BL23
- Kidney yang and qi deficiency, reinforcing: KD7, GV4, BL23
- Liver yin or blood deficiency, reinforcing: LV8, BL17, BL18
- Stomach yin deficiency, reinforcing: ST44, BL21
Auricular acupressure was included in the treatment protocol. Vaccaria ear seeds were applied to the following auricular acupuncture points:
- Shenmen
- Sympathetic
- Liver
- Kidney
- Lung
Patients were instructed to massage the points 15 minutes per day. At the end of all the sessions, patients were taught how to apply ear seeds for symptom management.
Acupuncture treatments were applied two times per week with a goal of 24 treatments over a 15 week period. Ten minutes were devoted to the TCM interview, 5 minutes for pulse and tongue evaluation, 10 minutes for insertion and obtaining deqi, and 30 minutes for needle retention.
Size 34 gauge needles with depths 0.25–0.5 inches were applied for most patients. Needle manipulation techniques (reinforcing tonification or reducing attenuation) were applied at the beginning of treatments and prior to removal of the acupuncture needles. To avoid discomfort, 40 gauge Seirin brand needles were applied to patients with sensitivity to needle insertion.
Conclusion
The researchers conclude that acupuncture is effective for the alleviation of PTSD. They add that current evidence supports additional research into the integration of acupuncture into PTSD patient care.
References:
[1] Hollifield, Michael, An-Fu Hsiao, Tyler Smith, Teresa Calloway, Tanja Jovanovic, Besa Smith, Kala Carrick et al. "Acupuncture for combat-related posttraumatic stress disorder: a randomized clinical trial." JAMA psychiatry (2024).
[2] Sinclair-Lian N, Hollifield M, Menache M, Warner T, Viscaya J, Hammerschlag R. Developing a traditional chinese medicine diagnostic structure for post-traumatic stress disorder. J Altern Complement Med. 2006 Jan-Feb;12(1):45-57.
[3] Sinclair-Lian N, Hollifield M, Menache M, Warner TD, Viscaya J, Hammerschlag R (2006) Developing traditional Chinese medicine diagnostic structure for posttraumatic stress disorder. J Altern Complement Med. 12:45–57.
[4] HollifieldM,Sinclair-LianN,WarnerTD, Hammerschlag R. Acupuncture for posttraumatic stress disorder: a randomized controlled pilot trial. J Nerv Ment Dis. 2007;195(6):504-513.


