Researchers tested the efficacy of acupuncture and herbal medicine for the treatment of diabetic peripheral neuropathy. All participants in the clinical trial were provided usual care. An observation group was provided additional therapeutics with acupuncture and Chinese herbal medicine. The addition of acupuncture and herbal medicine to usual care improved overall outcomes by 7.5% and the acupuncture and herbal medicine group had significantly greater outcomes for improvements in nerve conduction velocity. [1]
Diabetic peripheral neuropathy (DPN) is a long-term complication of diabetes, precipitated by elevated glucose or triglyceride levels, metabolic factors, and genetic traits. Exposure to high glucose levels over time injures peripheral nerves causing pain, tingling, numbness, throbbing, or burning sensations. In cases of diabetic polyneuropathy, both motor and sensory nerves are affected, thereby affecting sensations, strength, balance, and coordination.
Focal neuropathy affects specific nerves and can cause double vision, hearing disorders, inability to focus the eyes, back and pelvis pain, thigh pain, and abdominal pain. Neuropathy in the hands and feet is common and is often aggravated by the inability to heal from wounds caused by a lack of feedback from sensation. One clinical scenario that is more common than one may expect is that diabetics leave keys in their shoes and then wear them, causing extensive damage to the feet.
The research team devised a protocol that led to nerve conduction velocity and symptomatic improvement. They combined warm needle acupuncture and intake of Chinese herbal medicine. The herbal formula chosen for the study was Huang Qi Gui Zhi Wu Wu decoction. The researchers note that based on their data and existing research, the herbal formula helps to improve glucose and lipid metabolism and alleviate limb pain in patients with qi deficiency and blood stasis. They add that warm needle acupuncture improves nerve conduction velocity by reducing oxidative stress responses and promoting self-repair of neurovascular damage.
80 DPN patients from the Qianyang People’s Hospital of Gansu Province, diagnosed with qi deficiency and blood stasis syndrome, were selected for this study. They were divided into two groups, observation and control, with 40 patients each, using a double-blind randomized method.
Both groups received usual care: dietary control, exercise guidance, blood sugar control (oral hypoglycemic drugs like metformin, insulin injections if necessary), blood pressure management, and lipid regulation. The control group was given oral mecobalamin (vitamin B12) tablets (0.5 mg, three times a day) in addition to usual care.
The observation group received Huang Qi Gui Zhi Wu Wu Tang and warm needle acupuncture in addition to usual care. The prescription for Huang Qi Gui Zhi Wu Wu decoction included the following herbs:
- Huang Qi 9 g
- Bai Shao Yao 9 g
- Gui Zhi 9 g
- Sheng Jiang 18 g
- Da Zao 4 pieces
The formula was decocted in water to make 200 ml, taken warm morning and evening. Warm needle acupuncture was applied to the following acupoints:
- BL20 (Pi Shu)
- BL23 (Shen Shu)
- CV4 (Guanyuan)
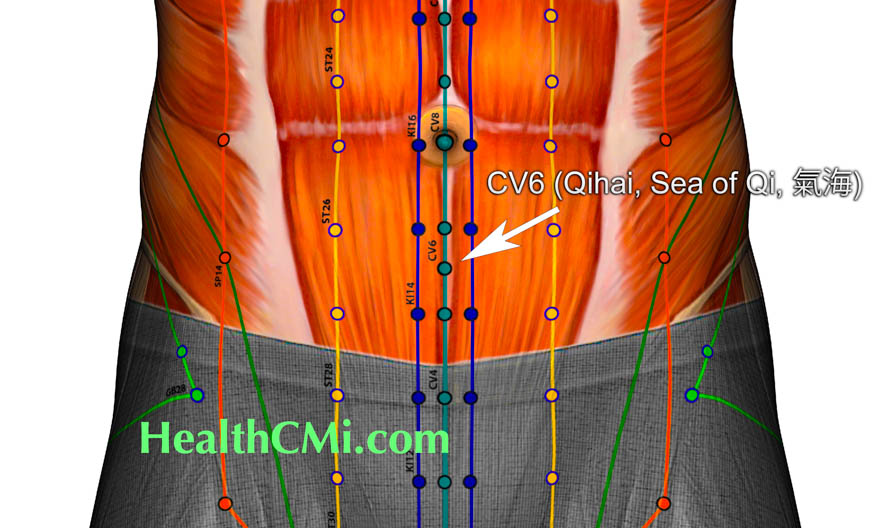
- CV6 (Qihai)
- ST36 (Zusanli)
- SP6 (Sanyinjiao)
- LI11 (Quchi)
- LV3 (Taichong)
- LI4 (Hegu)
The reinforcing- reducing technique was applied to the acupuncture needles. Moxibustion was applied after achieving qi, lit, and fixed to the needle handle using a 1–2 cm moxa stick. The duration of each needle retention was 15–30 min, according to the patient’s tolerance. Treatments were provided regularly for two weeks and a final evaluation of the indicators was performed after two months.
After treatment, both groups showed a significant improvement in overall scores, with the acupuncture and herbal medicine group outperforming the control group. Nerve conduction velocities increased notably post-treatment, with the acupuncture and herbal medicine group showing more significant improvements.
Symptom scores improved significantly after treatment, with the acupuncture and herbal medicine group demonstrating a more substantial decreases than the control group. The total effective rate of treatment was 95% in the acupuncture and herbal medicine observation group, which was higher compared with 87.5% in the control group. No significant adverse reactions occurred in either group during the treatment process. The researchers note that acupuncture and herbal medicine significantly improved clinical symptoms and signs, promoted nerve-self repair, reduced secondary nerve damage, improved nerve function recovery, and slowed disease progression.
Reference:
[1] Zhao Rong, Zhang Ding, Liu Yan, Wang Shan, Yuan Yuepeng & Zhang Mingbo. (2022). Clinical study on Huangqi Guizhi Wuwu Decoction combined with warm needle acupuncture in treating diabetic peripheral neuropathy (qi deficiency and blood stasis syndrome). Practical Traditional Chinese and Western Medicine Integrated Clinical Medicine (03), 5-9+34, 1671-4040.2022.03.002.


